How Do Medical Supplies Reach Disaster Zones?
When disaster strikes, the images that often dominate news coverage are those of collapsed buildings, flooded towns, or displaced families waiting in makeshift shelters. Behind these scenes, however, lies another story that is less visible but no less critical: the race to deliver medical supplies into disaster zones. Without the rapid arrival of bandages, antibiotics, vaccines, surgical kits, clean water, and basic equipment, the consequences of natural and man-made disasters would escalate into even greater humanitarian catastrophes. Getting medical supplies into disaster zones is far from straightforward. It is a complex, high-stakes endeavor that combines logistics, diplomacy, technology, and human resilience, operating under conditions where every hour matters and where the usual systems of commerce and infrastructure have often collapsed.
The process begins with assessment. Within hours of an earthquake, cyclone, epidemic, or armed conflict, humanitarian organizations and local authorities must determine what is needed most urgently. Needs assessments are carried out by rapid response teams who gather data from hospitals, clinics, and community leaders. The priorities can differ widely depending on the nature of the disaster. In the aftermath of earthquakes, trauma kits, orthopedic equipment, and surgical supplies are essential for treating crush injuries. After floods or cyclones, water purification tablets, mosquito nets, and diarrhea treatments often top the list due to the high risk of waterborne diseases. In conflict zones, emergency surgical kits, blood products, and burn treatments may be prioritized. Assessments feed into a supply chain system that mobilizes stockpiles pre-positioned by international agencies such as the World Health Organization, UNICEF, or the International Federation of the Red Cross and Red Crescent Societies.
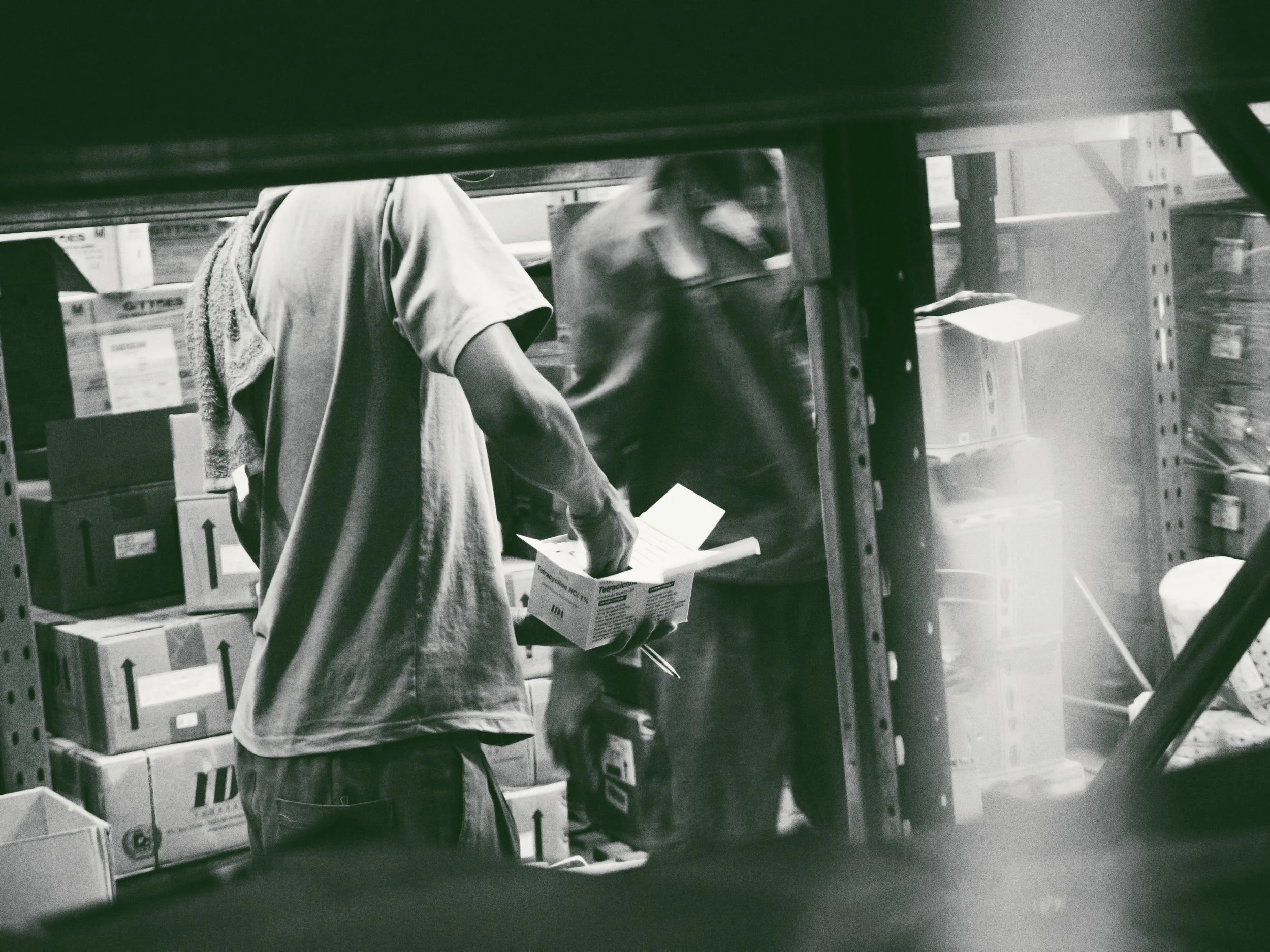
Stockpiles are a critical part of the answer to how medical supplies reach disaster zones. International agencies and NGOs maintain warehouses around the world, strategically located to enable rapid deployment. For example, humanitarian response depots in Dubai, Accra, or Panama are stocked with ready-to-ship supplies that can be flown out within hours of a request. These stockpiles include not just medical kits but also logistics essentials like tents, generators, and water systems. By having pre-packaged kits—such as the WHO’s Interagency Emergency Health Kits, which can support the basic health needs of 10,000 people for three months—response teams avoid the delays of sourcing items from scratch during a crisis. The existence of these depots allows supplies to move while assessments are still being finalized, buying crucial time.
Once the supplies are identified and mobilized, transportation becomes the central challenge. In many disaster zones, airports, seaports, and roads are damaged or overwhelmed. This creates bottlenecks at the very moment when speed is most critical. Air transport is often the first line of delivery. Cargo planes chartered by humanitarian organizations or militaries deliver pallets of supplies to the nearest functioning airport. In some cases, military airlifts provide the only means of reaching landlocked or isolated regions. Once on the ground, helicopters, trucks, or even boats take over for last-mile distribution. In extreme situations, when no infrastructure is usable, parachute drops of supplies are employed, though these carry risks of supplies being scattered or inaccessible. Each form of transport has its limitations, and coordination among multiple actors is essential to prevent duplication or wasted effort.
Customs and regulatory issues add another layer of complexity. Even during emergencies, medical supplies must clear customs and adhere to national regulations. This can cause significant delays if paperwork is incomplete or if governments insist on stringent checks. In some countries, bureaucratic hurdles have left shipments sitting idle in airports while patients go untreated. To mitigate this, international organizations often negotiate pre-disaster agreements with governments, creating “fast-track” procedures for humanitarian cargo. Diplomatic pressure and advocacy are sometimes required to ensure that lifesaving supplies are not delayed by red tape. Despite these efforts, regulatory barriers remain a recurring obstacle to rapid response.
Another dimension of supply chain management in disaster zones is coordination. Multiple actors are usually involved: national governments, international NGOs, UN agencies, local charities, and sometimes military forces. Without coordination, chaos can ensue, with duplication of some supplies and shortages of others. To address this, the humanitarian community employs a cluster system, in which different organizations take the lead on specific areas of response. The health cluster, coordinated by the World Health Organization, is responsible for overseeing medical supplies, ensuring that needs assessments are shared, and directing organizations to cover gaps rather than overlap. While coordination improves efficiency, it is not always perfect, and political or institutional rivalries can complicate efforts. Still, without it, supply chains would collapse under the weight of disorganization.
The last mile—the delivery of medical supplies from airports or warehouses to the actual communities in need—is often the hardest. Roads may be blocked by debris, bridges destroyed, or areas cut off by floodwaters. Armed groups or criminal gangs may control access, requiring negotiation or security escorts to allow passage. In these environments, local knowledge becomes indispensable. Community volunteers, local NGOs, and even individuals with motorcycles or donkeys often become the link between central supply depots and remote villages. In many cases, supplies handed over to local responders are distributed faster and more effectively than through large international convoys. Building partnerships with local actors is therefore not just a moral choice but a logistical necessity.
Technology has become an increasingly important tool in overcoming these challenges. During recent disasters, drones have been used to deliver small but critical medical supplies such as blood products, vaccines, or diagnostic samples to remote or inaccessible areas. Digital tracking systems provide real-time monitoring of shipments, helping agencies to identify bottlenecks and reroute supplies when necessary. Mobile apps allow health workers in the field to report shortages, which can then be addressed more quickly by central warehouses. These innovations, while not a panacea, offer valuable supplements to traditional supply chain methods, particularly in contexts where infrastructure is unreliable.
Funding, however, remains a constant constraint. Medical supply chains into disaster zones are expensive. Airlifts cost hundreds of thousands of dollars, and maintaining stockpiles requires continuous investment. Donor fatigue, competing global crises, and political considerations can leave humanitarian agencies scrambling for resources at the very moment demand spikes. Delays in funding commitments often translate into delays in supplies reaching the field. This financial fragility underscores the importance of long-term investment in preparedness, rather than relying solely on emergency appeals once disaster strikes. Preparedness not only saves time but also reduces overall costs by preventing the need for last-minute, high-cost logistics solutions.
The human element cannot be overlooked. Delivering medical supplies into disaster zones depends on people willing to work in dangerous, exhausting, and emotionally taxing environments. Logistics officers, warehouse staff, truck drivers, and health workers all play critical roles, often risking their own safety to ensure supplies reach those in need. Their work is complicated by stress, fatigue, and in some cases direct threats from hostile actors. Yet without their persistence and courage, even the best-stocked warehouses and most advanced technologies would be useless. The resilience of these individuals, often drawn from both international organizations and local communities, forms the backbone of disaster medical supply chains.
Ultimately, the question of how medical supplies reach disaster zones is answered not by a single system but by a tapestry of interlocking efforts. Pre-positioned stockpiles, international airlifts, local volunteers, digital tools, and diplomatic negotiations all combine to form fragile but effective chains of delivery. Each link in the chain carries its own vulnerabilities—an airport closure, a customs delay, a funding gap, or a broken road—but when the system works, lives are saved and communities are stabilized. The challenge lies in strengthening these chains before disasters strike, ensuring that speed and efficiency are built into the system rather than improvised under duress.
Disasters, whether natural or man-made, are inevitable. What determines their human impact is how prepared we are to respond. Medical supply chains are one of the most critical determinants of survival in the aftermath of crisis. They ensure that a child with pneumonia can breathe, that a wounded survivor can receive surgery, and that an outbreak of disease can be contained before it spreads. The complexities are immense, but the stakes are higher still. By investing in systems, technology, and cooperation, and by valuing the role of local communities alongside international actors, the world can ensure that when the next disaster strikes, medical supplies will not be a distant hope but an immediate reality.